Throughout dental literature related to the treatment of TMD, the modality that is advocated nearly universally is the use of occlusal appliances, commonly referred to as “splints”. A wide variety of designs of occlusal appliances are known to be useful and effective in the treatment of most TM disorders. A number of theories have been suggested as to why occlusal appliances are effective in reducing the symptoms associated with TMDs, however the mechanisms that are involved have not yet been scientifically documented. Many experienced and respected clinicians, over many decades, have made similar observations and have come to similar conclusions regarding the effectiveness of occlusal appliances. Regardless of how consistent the clinical experience may be, without sufficient scientific data to support any of these theories, conclusions based on clinical observation alone must still be considered “anecdotal”.
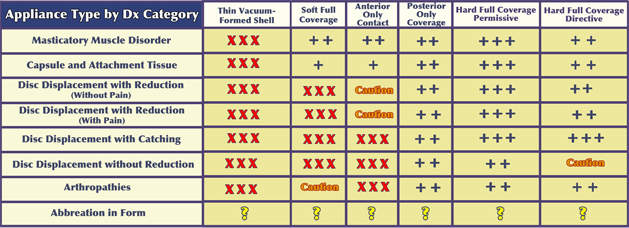
The following table of recommendations for Appliance Type by Diagnostic Category is based upon the clinical experience of Drs. Higdon and Howard.
Any plastic device that is placed between the teeth, regardless of its design or the material of which it is made, alters the occlusal environment in some way. The consistency of the observations of respected clinicians implies that favorable physiologic adaptation is responsible for producing favorable improvement. Understanding these physiologic mechanisms, based on a biologically-specific diagnosis of the individual patient’s presenting condition, is the basis for consistent effective use of occlusal appliances. It is essential to avoid hit-and-miss, trial-and-error “appliance therapy” that too commonly occurs as a result of inadequate understanding and training. We must ask ourselves, “What is the disharmony within the masticatory mechanism that needs to be altered to achieve the desired treatment objectives?”
Some patients will state, “I’ve tried ’splints’ and they haven’t worked”, meaning “Don’t tell me that you want to do that to me again.” A common misperception, not only on the part of some patients and insurances companies but surprisingly on the part of quite a few dentists, is that if the patient has ever been fitted with a piece of plastic in their mouth, they have had effective splint therapy. There is no magic in the plastic itself and an intraoral appliance is no more than a tool that requires knowledge, skill, and experience to achieve a quality outcome.
If the major problem to be addressed is predominantly muscular in nature, without a significant involvement of the temporomandibular joints, then we need to understand which appliance design can produce a positive muscular response. If, on the other hand, the problem that needs to be addressed involves the temporomandibular joints, one needs to know as specifically as possible what the diagnostic category of that joint condition is to be able to decide on an appropriate design for the appliance. It should be mentioned that when there is a significant joint component to the problem, there will almost always be a muscular component that must also be addressed. So in appliance design, the muscular component must always be considered.
In most cases, problems that involve primarily the muscles are relatively easy to address. Once the joints have become a part of the problem, the level of challenge increases and it becomes extremely important to appreciate the degree of joint involvement. On the low end, it may involve apparently uncomplicated clicking and popping without pain. However, even painless clicking does tell us something about the structural condition of the joint(s) and should not be treated as inconsequential when selecting an appliance design. (See TMJ Anatomy in the navigation menu)
When clicking and popping of the TMJs is accompanied by pain arising from the joints, the clinician must then consider what in the design of the occlusal appliance will most effectively address the joint pain as well as the inevitable reflex muscular splinting and pain that will accompany it.
If the patient is describing catching of one or both joints, whether or not there is pain from the joints, the TMJ dysfunction has now escalated to an even more critical phase. (See Diagnosis —> Diagnostic Categories —> Variability, Progression and the Critical Zone) Catching can progress to locking, sometimes very quickly. Therefore, addressing the catching at an early stage becomes quite important. In this instance, further consideration of appliance design and how much the appliance is to be worn by the patient become even more critical. Certain types of appliances, such as anterior deprogramers, the B splint, and the NTI, are clearly contraindicated for catching joints and can actually contribute to the joint progressing to locking.
Regardless of the presentation of the patient’s problem, the best clinical judgment results from a thorough history and a careful examination and sometimes sophisticated imaging. Shooting from the hip in selecting an appliance design, without a careful assessment and a reasonable biologically-specific diagnosis, can lead not only to a lack of improvement but the potential for a problem actually worsening, perhaps as a result of an inappropriate treatment choice.
A complete description of the use of occlusal appliances is well beyond the scope of this website. Please download "Why Splints Work (and why they may not)", below. We also recommend Chapter 15 in Okeson’s text and Chapter 32 of Dawson’s text, as well as other Textbooks.