Sophisticated imaging techniques of the temporomandibular joints are not indicated for every patient. The need for specialized imaging should be based on a careful history and examination, and then completed only when there is reason to believe that imaging will guide the appropriate treatment. If the clinical presentation is suggestive of an internal derangement, a very reliable diagnosis can usually be made by a thorough history and examination, without specialized imaging.
Diagnosis of some conditions that affect the TMJ cannot be made by means of history and clinical examination alone and imaging may be indicated. These include congenital and developmental malformations of the mandible and/or cranial bones, and acquired disorders, including neoplasia, fractures, dislocations, ankylosis, and disc displacement, as well as inflammatory diseases and a wide range of arthritides.

Screening Imaging of the Temporomandibular Joints
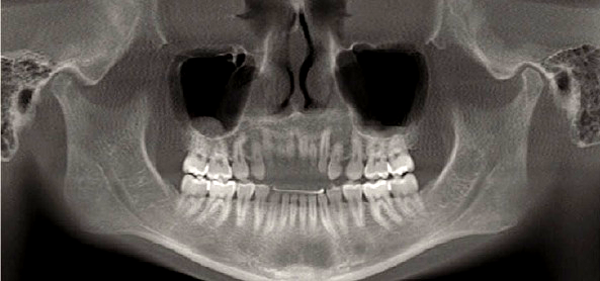
A screening image, typically a panoramic radiograph, permits assessment of the form of the condyle and the integrity of the cortex and is an important adjunct to the initial history and examination. An additional benefit of a panoramic image is the ability to visualize other structures in the maxillofacial region. In a panoramic image the condyles are intentionally brought down and forward in the fossae by having the patient protrude the mandible, but the condyles may still be partially obscured by adjacent bony structures.
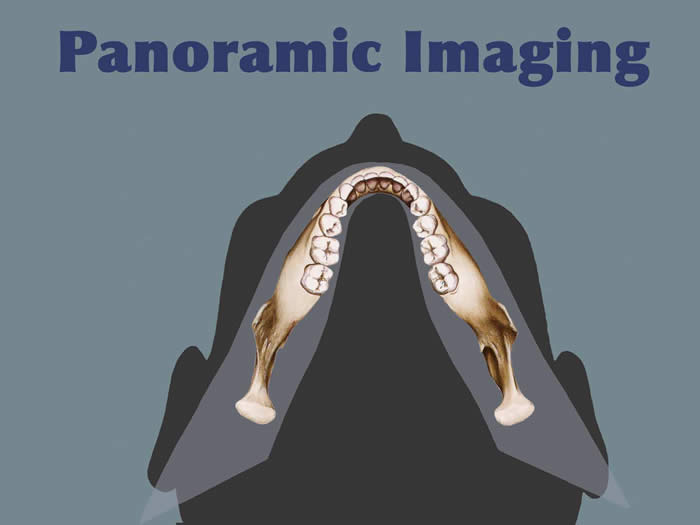

With the advent of cone beam CT (CBCT) imaging, it is now possible to acquire a panoramic image with the teeth together, thus making it possible to see the condyles in their relationship to their fossae.
Because conventional panoramic imaging is still more common still more commonly available in dental offices than is CBCT, and because a conventional panoramic exposes the patient to less radiation than a CBCT scan, the conventional panoramic is the preferred choice as a screening image for most TMD patients.

Plain Film Radiography
Plain Film Radiography
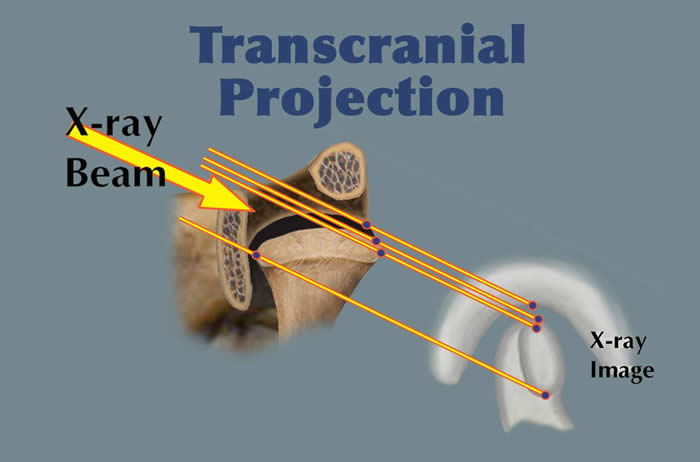
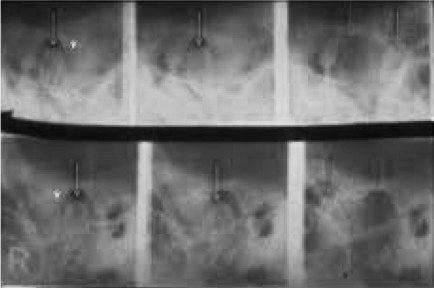
Plain film radiography refers to images made with a stationary x-ray source and depicts only mineralized parts of the joint. These techniques include transcranial,transpharyngeal, transmaxillary, and submental-vertex views.
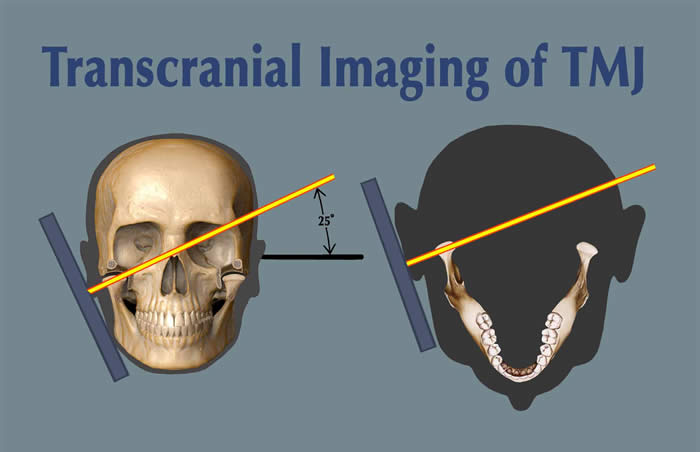
Transcranial Viewt
The transcranial view does not project a true sagittal image of the condyle, fossa, or joint space. Because of the distortion that results from the angle of the x-ray beam to these joint structures, this projection has largely been abandoned in favor of more accurate and revealing projections. Historically, one of the advantages of the transcranial projections has been that it could be taken in the dental office.
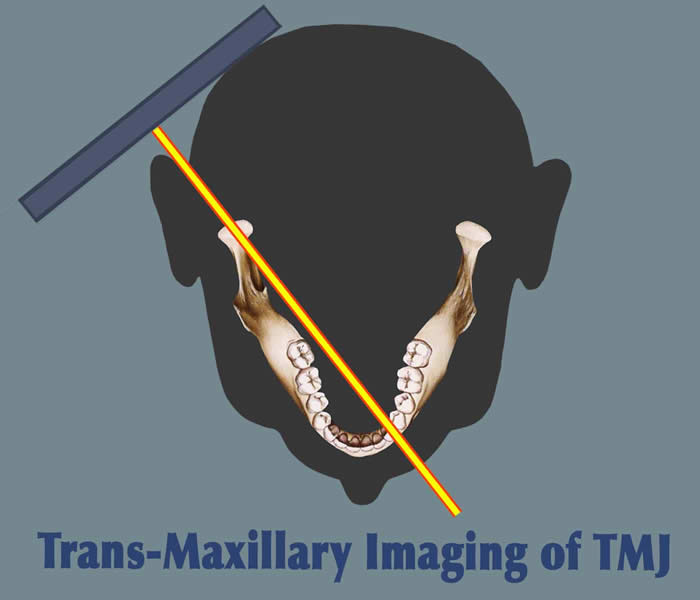
Transmaxillary View
This is a modified anterior-posterior projection that produces an image that is perpendicular to the long axis of the condyle. It is taken with the mouth wide open which positions the condyle at the height of the tubercle to avoid superimposition of the condyle onto the base of the skull while simultaneously allowing the x-ray beam to be tangent to the inferior surface of the eminence and the superior surface of the condyle. This view is useful in trauma patients for identifying fractures of the condylar neck that might not show up on a panoramic image.

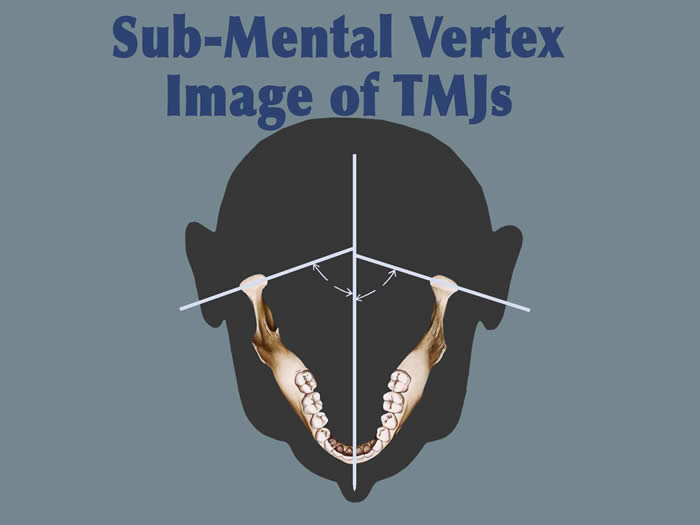
Submental-vertex View
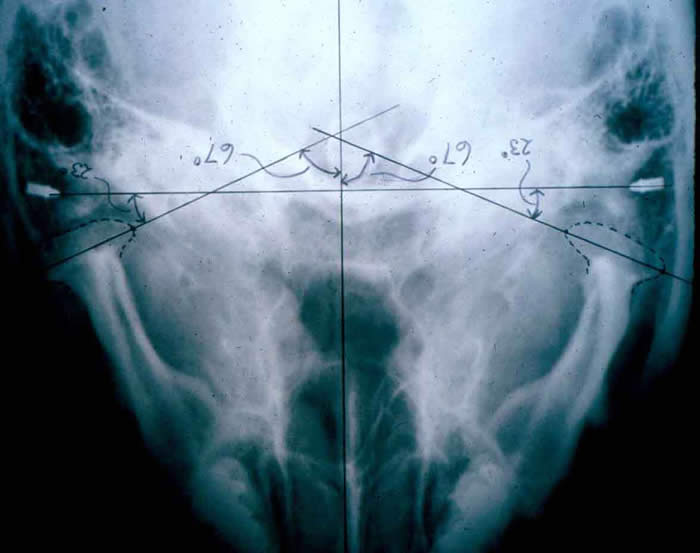
This projection allows measuring the angle of the condyles to the mid-sagittal plane. It is often used as a scout film prior to taking corrected tomograms, thus permitting accurate sectioning of the condyles perpendicular to their individual long axes.
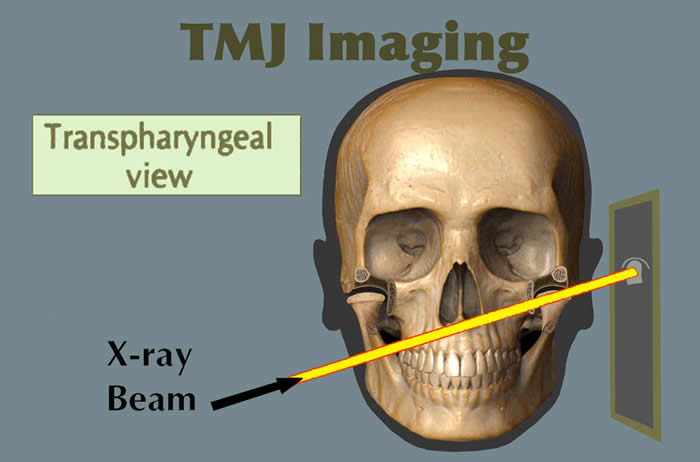
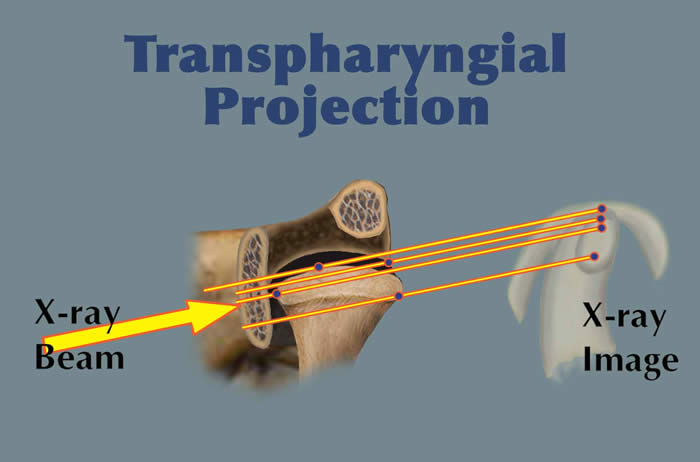
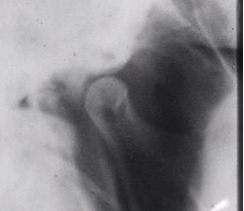
Transpharyngeal View
This view is a projection of the TMJ through the opposite side sigmoid notch. The mouth must be open to avoid superimposition of neighboring structures. This view is useful for demonstrating destructive changes of the condyle and may be of value in diagnosing fractures of the condylar neck. The reverse Towne's projection is also for detecting condylar neck fracture.
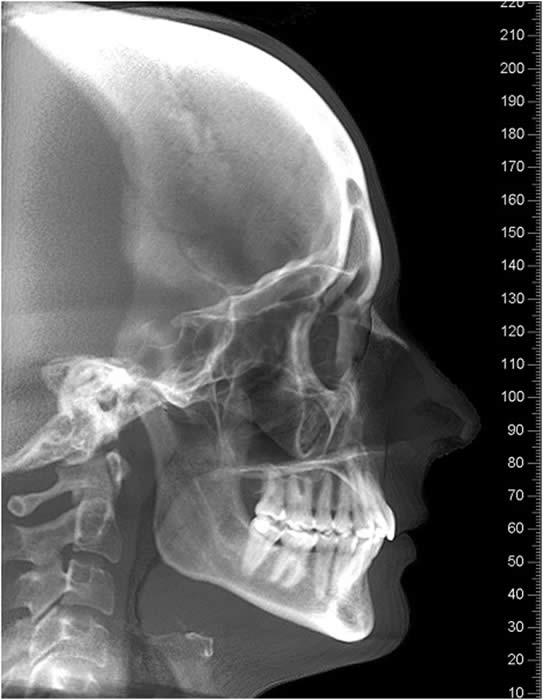
Other Plain Film Views The lateral cephalogram and the posterior-anterior cephalogram are routinely used by orthodontists and are useful in assessing skeletal relationships and facial asymmetry but are not of value for information about the TMJ diagnosis because of superimposition .

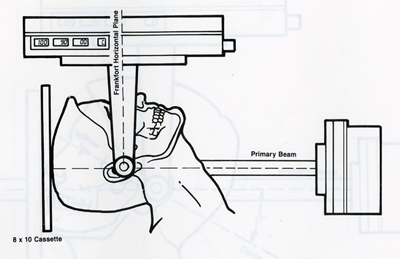
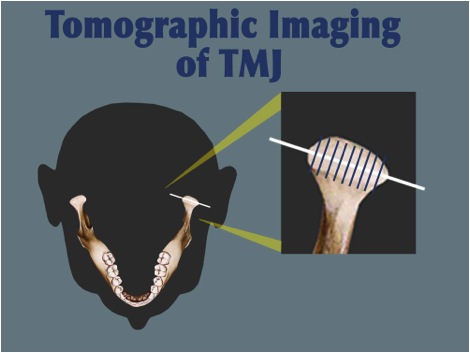
Conventional Corrected Tomography
Tomography of the temporomandibular joints makes possible multiple parallel sections through the region of interest without superimposition of other structures. The disadvantage is the inability to visualize soft tissue, thus not providing reliable information about disc position or form. With the aid of information obtained from a submental-vertex projection, corrected tomographic sections can be obtained that are perpendicular to the long axis of each condyle, even though the angles of the condyles may differ from side to side in an individual patient. The advantage of corrected tomography is the increased accuracy of the spatial relationship of the condyle to the fossa, make right to left side comparison of condylar size and shape, and evaluate the slope, height and integrity of the tubercle.

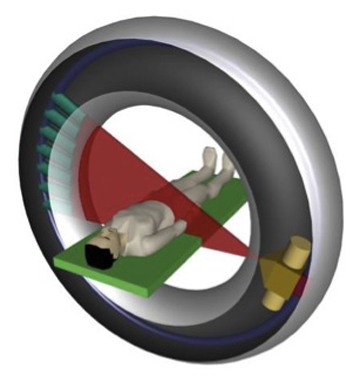
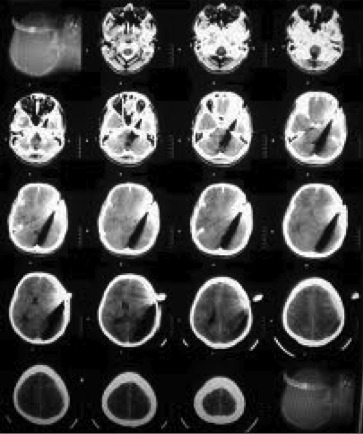
Hospital-Based Computed Tomography (CT)
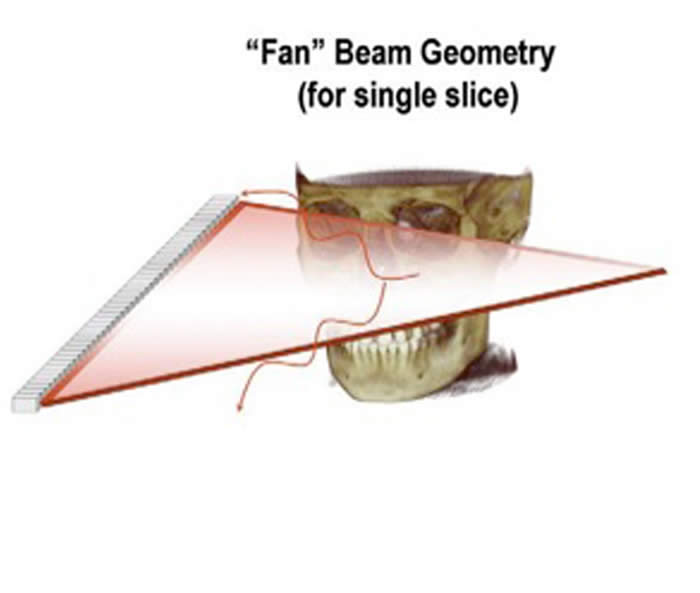
Computed tomography (CT) uses a narrowly collimated beam of x-rays that rotates in a full arc around the patient to produce an image of detailed cross-secional slices. A major advantage of CT is its ability to image bone, soft tissue and blood vessels all at the same time. An array of detectors, positioned at several angles, records those x-rays that pass through the body. The image is created by a computer that calculates tissue absorption and can produce three dimensional reconstructed images representing tissues that demonstrates the densities of the various structures. CT is less sensitive to patient movement than MRI. CT can be performed if you have an implant medical device of any kind, unlike MRI.
Tumor masses, infarctions, bone displacement, and accumulations of fluid may be detected. It is useful for the diagnosis of bony abnormalities including fractures, dislocations, arthritides, ankylosis, and neoplasia. Three dimensional reconstructed images can be produced.


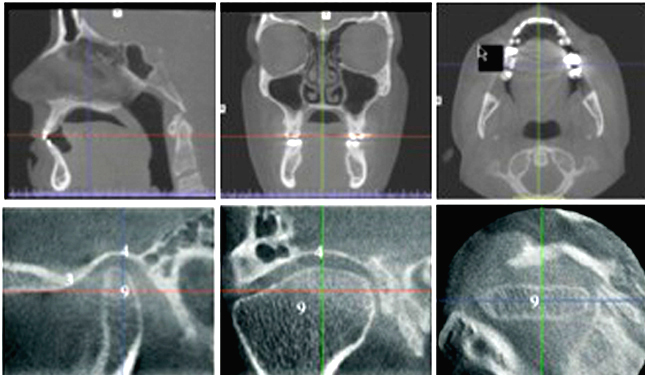
Cone Beam Computed Tomography (CBCT)
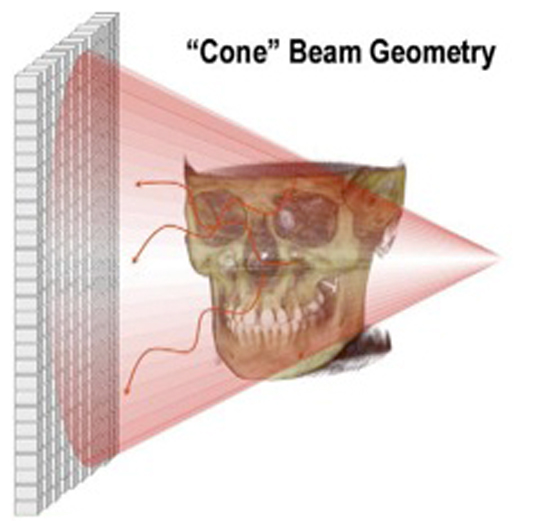
Cone beam computed tomography (commonly referred to by the acronym CBCT) is a medical imaging technique consisting of X-ray computed tomography where the X-rays are divergent, forming a cone.
CBCT has become increasingly important in diagnosis and treatment planning in implant dentistry, among other things. Perhaps because of the increased access to such technology, CBCT scanners are now finding many uses in dentistry, such as in the fields of endodontics and orthodontics, as well.
During a CBCT scan, the scanner rotates around the patient's head, obtaining up to nearly 600 distinct images. The scanning software collects the data and reconstructs it, producing what is termed a digital volume composed of three dimensional voxels of anatomical data that can then be manipulated and visualized with specialized software.








Arthrography
In the past, arthrography and arthrotomography, contrast-enhanced imaging, have been considered the methods of choice for imaging TMJ internal derangement. Contrast media is injected into one or both joint spaces under fluoroscopic guidance. The intra-articular tissues (disc and retrodiscal tissues) are then “silhouetted” by the contrast material, allowing visualization of the disc profile, as well as real-time movement of the condyle with respect to the disc within the joint. This is the major advantage of this technique. It can also demonstrate perforations of the tissues that are recognized under fluoroscopic observation when injection of contrast into one space then flows into the other. It also allows visualization of disc adhesions. Its limitation is that it does not allow interpretation of sideways or rotational displacements of the disc.
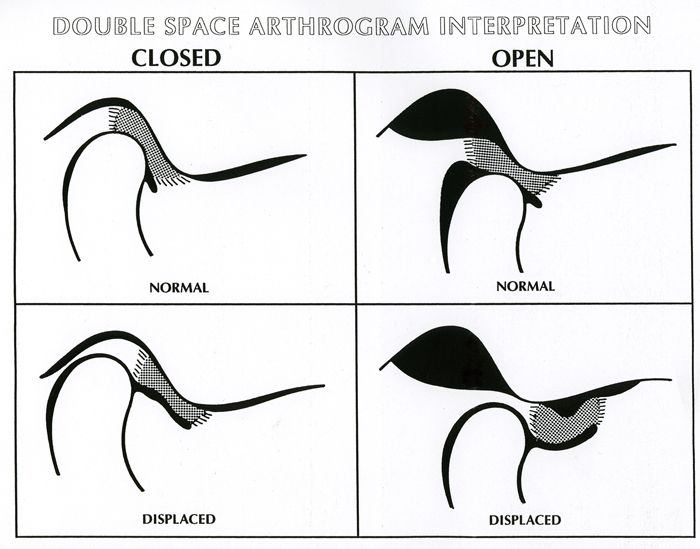
A disadvantage of this technique is that it is an invasive procedure (needle injection of contrast) and because there are infrequent allergies to the contrast material. It is also a technically demanding procedure, requiring skill and experience to produce consistent quality studies.

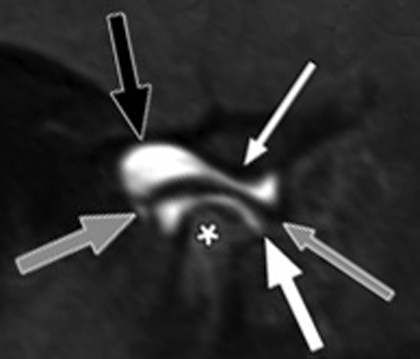
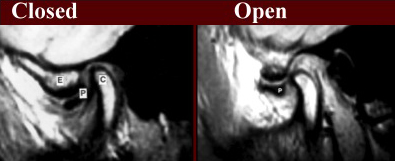
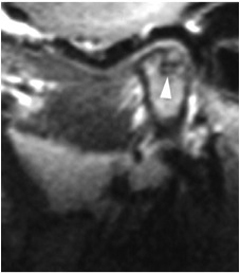
Magnetic Resonance Imaging
This imaging method has become the default “gold standard” for imaging of internal derangements of the temporomandibular joints. Major advantages include the fact that it is non-invasive and does not use ionizing radiation to produce images. It is also able to demonstrate sideways and rotational displacements. It is capable of producing only still images (open and closed), not real-time movement studies, and in that respect it has a significant disadvantage compared to arthrography.
MRI is contraindicated in patients who have been fitted with a pacemaker, have intracranial vascular clips, and metal particles in the eye or other vital structures, due to the strength of the magnetic field. Other contraindications for MRI can include obesity, claustrophobia, or inability to remain motionless for the examination, which can take several minutes to complete.









Other Imaging Techniques
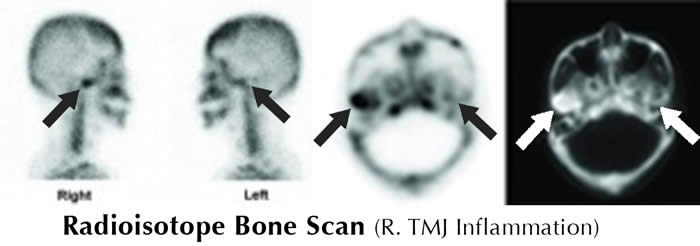
Single-photon emission computed tomography (SPECT), radioisotope scans, ultrasound, and thermography have been used to evaluate the TM joints. SPECT and radioisotope scans are particularly sensitive for inflammatory disorders and arthritides but are not specific for these conditions. Thermography has been used experimentally and may have a role in detecting joint inflammation. Ultrasound is not considered to be sensitive or specific for any TMJ abnormality.

Imaging Protocol
As previously stated, the selection of appropriate imaging of the temporomandibular joints should be based on a thorough history and examination. Imaging should not be considered the primary basis for diagnosis but should supplement the clinical evaluation, when indicated. Selection of imaging should be based on what technique will provide the desired information at the lowest cost and least radiation.
For example, when hard tissue imaging of the TM joints is indicated, tomography will be less costly and will expose the patient to less radiation than will conventional CT. However, with the advent of CBCT, radiation exposure is considerably less than conventional CT and particularly with the potential to view the selected structures from any angle, this option has become a reasonable choice for imaging hard tissue. Unfortunately, CBCT cannot provide imaging of the articular disc.
Developmental Disorders
Facial asymmetry, especially progressive asymmetry, suggests development disorders such as condylar aplasia, hypoplasia, or hyperplasia. Hard tissue imaging is indicated and CBCT is now the optimal choice for diagnosing such conditions. Because disc derangement may cause facial asymmetry in young persons, MRI may also be appropriate in some cases. Both hard and soft tissue imaging may be required when facial asymmetry is thought to be related to juvenile rheumatoid arthritis affecting the TM Joints.
Disc Derangements
In individuals who demonstrate non-symptomatic clicking or popping of the TM joints, particularly when the individual does not wish to consider any treatment, no imaging is indicated. An explanation to the individual of the cause of these joint sounds is usually appropriate, with a particular caution that sometimes simple clicking and popping can progress to catching or locking.
If the individual reports any progression in the direction of catching or locking, treatment is more likely to be an appropriate consideration, even in the absence of specific joint pain. In this instance, imaging may be indicated, particularly if the dysfunction does not respond to conventional conservative treatment. In such instances, soft tissue imaging of the joints would be appropriate and MRI would be the method of choice.
TMJ Dislocation
Dislocation of the mandibular condyle out of the glenoid fossa may require hard tissue imaging. Here, again, CBCT would not only permit visualization of the condylar position but would also permit evaluation for possible fracture or the presence of foreign objects.
Inflammatory Disorders
When an inflammatory disorder, such as various arthritides, is suspected, hard tissue imaging is recommended and CBCT will be a good choice. However if the suspected differential diagnosis includes disc derangement or rheumatic disease, MRI may also need to be considered.
Ankylosis
When fibrous or bony ankylosis is suspected, hard tissue imaging is recommended. Here, again, CBCT will prove very appropriate.
Fracture
When a condylar fracture is suspected, particularly when there may be extensive facial fractures or complex fractures of the TMJ, CBCT will be an appropriate choice, although mandibular fractures, including condylar fractures can often be seen well on a panoramic image.
This information is intended to provide only an overview of the use of imaging in the diagnosis of disorders of the temporomandibular articulation and the surrounding structures.





