| |
|
 |

“The use of symptomatology rather than objective clinical means of defining TMD is ultimately a reflection of our limited appreciation of the pathophysiological mechanism underlying these conditions. . . . Success in treating disease requires first an ability to accurately and reliably diagnose the underlying pathosis”
– Dimitroulis et al., 1995
A common misperception, perpetuated by usage in popular media, is that the term “TMJ” represents a distinct, well-defined disorder and that all patients who have “TMJ” are the same or very similar. Within the dental profession that misperception is gradually being dispelled but most dentists continue to lack a clear understanding of how patients with temporomandibular disorders (TMDs) actually do differ.
Temporomandibular disorders occur as a continuum, from relatively minor disturbances of masticatory muscle function (without involvement of the temporomandibular joints) to major structural and functional disturbances of the TM joints. In addition to the muscles of mastication, there is often an involvement of other muscles of the head and neck as well.
Across this continuum, the indications for treatment can also vary a great deal, from no treatment at all at the one end, to surgery of the TM joints and subsequent orthopedic rehabilitation of both joint and muscle function at the other end. For the majority of these disorders, non-invasive therapies are typically effective in significantly reducing the major symptoms and can often also contribute to a restoration or improvement of physiologic function of the masticatory apparatus. How can we divide this continuum, as patients appear clinically, to assure that treatment is provided only when indicated and is appropriate to the condition? See Variability, Progression, and the Critical Zone, below.
To assure optimum outcomes, appropriate treatment must be based on clearly defined treatment objectives that are consistent with a biologically-specific diagnosis in each patient. Generic “TMJ” treatment, without understanding the actual nature of the underlying problem, is never appropriate.
The following diagnostic classification is proposed as a basis for arriving at appropriate clinical decisions.

Patient Type 1
Masticatory Muscle Disorders
Masticatory muscle disorder include myalgia, myositis, or myofascial pain (MFP). Myalgia is objective pain within a muscle; myositis is acute, constant pain with generalized inflammation and swelling of a muscle with pain that usually increases with mandibular movement. Myofascial pain (MFP) is dull, aching regional pain that is referred from or emanating around active trigger points (localized tender points) in muscle, tendon, or fascia.
Findings from Screening History and Screening Exam
• Muscle pain (myalgia) with or without muscle dysfunction.
• No historical, clinical, or imaging evidence of structural alteration of the TM joints.
(A screening panoramic film, or other joint imaging, with good visualization of the TM joint condyles is desirable but not essential)
– No joint sounds (click/pop, or crepitation).
– No history of joint sounds.
– No joint pain with palpation, joint loading, or with provocation testing.
Primary Objective of History and Examination
• To rule out joint sounds (click/pop, crepitation), pain or dysfunction, thereby ruling out any involvement of the TM joints.
Caution: A locked joint may not produce any joint sounds. Therefore, also look for evidence of altered range of motion.

Patient Type 2
Capsular and Attachment Tissue Disorders
(Joint Sprain and/or Joint Hypermobility Disorders)
Capsulitis or synovitis refers to inflammation of the capsular or synovial lining of the TMJ capsule, ligaments or disc attachments. This includes localized pain at rest that is exacerbated with function and loading of the TM joint. This category also includes systemic ligament laxity, which can contribute to joint hypermobility and instability.
Findings from Screening History and Screening Exam
• TMJ pain with movement and/or with lateral palpation.
• No historical or clinical, evidence of joint structural change (click, pop, crepitation).
• With hypermobility disorders, late-opening pops may occur and are likely to be subluxation and not a disc interference click/pop.
• This type of joint pain is typically accompanied by masticatory muscle splinting and possible muscle pain.
(A screening panoramic film or other joint imaging with good visualization of the TM joint condyles is desirable but not essential)
Primary Objective of History and Examination
• To rule out joint sounds (click/pop, crepitation), or joint dysfunction. If disc-interference joint sounds are present, this would indicate a disc displacement and would therefore be a Type 3, not a Type 2.
• This type does not include infectious diseases. TMJ infections are uncommon but should be considered as a possibility.
Caution: A locked joint may not produce any joint sounds. Therefore, also look for evidence of altered range of motion.

Patient Type 3
Disc Displacement with Reduction – No Joint Pain
(minimal or no disc interference)
There are several types of internal derangements or disc displacements, including those that progress to disc interference disorders with catching and locking of the joint.
Findings from Screening History and Screening Exam
• Evidence (historical or clinical) of TM joint structural change (click, pop, crepitation).
• No joint pain during function, or with palpation, loading, or provocation testing.
• With or without muscle pain and/or dysfunction (In the absence of joint pain, there may be muscle tenderness to palpation, or a subjective awareness of muscle pain. Muscle pain typically results from prolonged or excessive muscle contraction, for any of several reasons.)
• No history or clinical signs of disc interference (catching or locking).
(A screening panoramic film or other joint imaging with good visualization of the TM joint condyles is desirable but not essential. However, absence of condylar change does not rule out this type.)
Primary Objective of Examination
• To rule in or rule out joint pain and to be sure that the disc displacement is not contributing to problematic joint dysfunction, i.e. disc interference, such as catching or locking that may represent a progressive clinical problem. Careful questioning of the patient regarding catching of one or both joints is critical. If there is joint pain, this would be a Type 4 patient, not a Type 3. If catching is present, whether or not there is pain, this would be a Type 5, not a Type 3 or4.

Patient Type 4
Disc Displacement with Reduction – With Joint Pain
(minimal or no disc interference)
There are several types of internal derangements or disc displacements, including those that progress to disc interference disorders with catching and locking of the joint.
Findings from Screening History and Screening Exam
• Evidence (historical or clinical) of TM joint structural change (click, pop, crepitation).
• Joint pain during function, or with palpation, loading, or provocation testing.
• With or without muscle pain and/or dysfunction (Muscle pain typically results from prolonged or excessive muscle contraction, for any of several reasons. When joint pain is present, there will typically be muscle pain in response to the joint pain; i.e. co-contraction or muscle splinting. Therefore, however, co-contraction or muscle splinting may not be the only source of excessive muscle contraction.).
• No history or clinical signs of disc interference (catching or locking).
(A screening panoramic film or other joint imaging with good visualization of the TM joint condyles is desirable but not essential. However, absence of condylar change does not rule out this type.)
Primary Objective of Examination
• To rule in or rule out joint pain and to be sure that the disc displacement is not contributing to problematic joint dysfunction, i.e. disc interference, such as catching or locking that may represent a progressive clinical problem. Careful questioning of the patient regarding catching of one or both joints is critical. If there is no joint pain, this would be a Type 3 patient, not a Type 4. If catching is present, whether or not there is pain, this would be a Type 5, not a Type 3 or4.

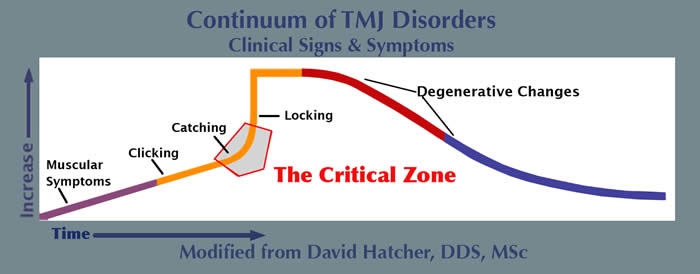
Variability, Progression, and the Critical Zone
Disc displacement with reduction is an extremely common phenomenon. Studies using history and exam only have demonstrated that between 30 - 40% of the general population has clicking and popping of the TM joints. This finding is nearly always indicative of a disc displacement. In studies that have also used MRI imaging on general population groups (non-patients), the prevalence rate increases to somewhere around 75 – 80% of the general population, with women represented more frequently than men. It is fortunate that most of these individuals do not seek nor need treatment and seem to go on through life with this condition. Most apparently go to their grave with it.
This frequency of occurrence, however, can easily lead to complacency about a finding of sounds from the TM joints. A Type 3 patient (clicking/popping without joint pain) may require no treatment whatever, so long as there is no indication of catching. This would certainly be the most common scenario. If joint pain is absent but there is muscle pain, treatment would be much like with a Type I TMD. However, mild clicking and popping that is progressively getting louder, in spite of an absence of pain, is almost certainly indicative of a condition that is progressing and may either become painful (Type 4) or, more likely, may progress to catching (Type 5). Therefore, even in the absence of joint pain, when there is evidence of this type of progression, appropriate early intervention is advisable.
A Type 4 patient who demonstrates clicking/popping together with pain from the TM joint(s) will also benefit from a stabilization appliance that provides the potential for re-posturing of the mandible, as described above. So long as there is no evidence of catching (Type 5), most Type 4 patients will respond very well to appropriate occlusal appliance therapy. Changes in joint position will occur commonly with Type 4 patients and attention to this and the possible need for occlusal management must be kept in mind when undertaking treatment of these patients.
It should be quite apparent that treatment of a Type 4 patient requires not only some careful questioning (is clicking, popping, catching progressing?), but also a fairly simple but critical examination for joint pain. This is where the screening procedure really begins to pay off (see “Early Recognition of Temporomandibular Disorders”).
The Critical Zone
This term is used to designate an area in the continuum of TM disorders that can rapidly move from risk-free to high-risk conditions. Being able to determine whether a patient’s TM disorder has entered the Critical Zone requires that the patient be carefully screened by means of the screening history and the screening exam. If this has not been done, the patient can appear to have a relatively minor condition but the condition can potentially worsen very quickly with very unfavorable outcomes.
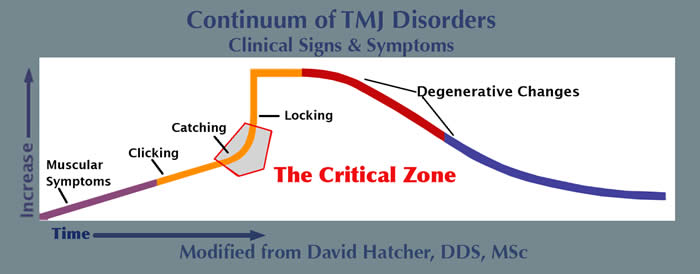
Inappropriate treatment may accelerate this progression. In discussing Type 4, above, if the clicking/popping involves even mild catching, or if the clicking/popping has been getting progressively more frequent or louder over time, this is evidence of progression and the joint condition may rapidly move from Type 4 to Type 5 (catching) or even to Type 6 (locking) if the wrong approach to treatment is undertaken. A Type 4 patient may be in the Critical Zone, in spite of an absence of joint pain.
The significant point that needs to be understood is that if the dentist decides to treat a Type 4 patient, they need to be very sure that there is little chance that the treatment will not promote a progression to a more advanced condition. That having been said, if appropriate treatment is provided, it is fairly unlikely that the patient’s condition will worsen.

Patient Type 5
Disc Catching with Reduction
(with or without pain)
Findings from Screening History and Screening Exam
• The primary historical and clinical feature is catching but without locking.
• Evidence (historical or clinical) of TM joint structural change (click, pop, crepitation).
• With or without muscle pain and/or dysfunction (when joint pain is present, there will typically be muscle pain, as well, in response to the joint pain; i.e. co-contraction or reflex muscle splinting).
• Possible TM joint pain with palpation, loading, or provocation testing in one or both joints.
(A screening panoramic film or other joint imaging with good visualization of the TM joint condyles is desirable but not essential. However, absence of condylar change does not rule out this type.)
The Primary Objective of History and Examination
• To determine the potential for disc interference (catching) to progress to a more problematic condition.
Patient Type 4 — Variability
Catching Presents Along a Continuum:
• Grade I Catching: Patient reports brief interference with mandibular movement that is easily overcome with minor lateral jaw movement.
• Grade II Catching: Interference is somewhat more problematic but is still overcome fairly easily.
• Grade III Catching: Typically described as intermittent brief locking. Requires more effort to overcome.
The Primary Objective of the Screening History – Questions to Ask the Patient
• How long has the patient been aware of catching?
• Has the catching stayed the same over time or been getting worse? (i.e. catching more or more difficult to overcome?).
The answers to these questions will suggest whether this condition is progressing. When progression is suggested, management must be specific to the condition in an attempt to intercept this tendency to progress.

Patient Type 6
Disc Displacement without Reduction
(Joint locking)
Disc interference with locking (non-reducing disc displacement NRDD) is usually accompanied by a significant alteration in the form of the displaced articular disc. In the acute phase there is limited mandibular range of motion and deflection of the mandible to the ipsilateral side on opening. With chronic NRDD, the opening range of motion, with time, often returns to near normal with minimal or no deflection on opening. As opening increases, the deflection is more likely to be seen at the end-range of the opening movement.
Findings from Screening History and Screening Exam
• Locking, as indicated by history, clinical signs, and/or imaging.
– With or without joint pain.
– With or without muscle pain (when joint pain is present, there will typically be muscle pain, as well, in response to the joint pain; i.e. co-contraction or reflex muscle splinting).
– Joints that have locked have typically passed through Type 5. However, the patient may be unaware that catching had preceded the locking.
Locking can also occur acutely in response to trauma, without being preceded by catching. Chronic locking, based on clinical findings, such as moderately decreased range of motion, is sometimes seen without any awareness on the part of the patient.
• Joint locking may have an acute onset (recent — hours to days).
Typically, with acute onset, range of motion will be restricted.
• Joint locking may be chronic (occurring months or years previously).
The patient may be unaware that it occurred. Not uncommonly the current range of motion may approach normal.
(A screening panoramic film or other joint imaging with good visualization of the TM joint condyles is desirable but not essential. However, absence of condylar change does not rule out this type.)
The Primary Objective of History and Examination
• To determine the degree that locking, with or without pain, is interfering with normal function.
• The patient’s age, degree of pain, difficulty with function, both now and potentially in the future, may influence treatment decisions.

Patient Type 7
TMJ Arthropathies
Osteoarthritis (OA) and other arthropathies are characterized by crepitus and may be a result of progression of disc displacement disorder, may be secondary to an inflammatory process, or may be just the natural history of aging to the TM joint.
Findings from Screening History and Screening Exam
• Early changes, often involving primarily soft tissues, may not be evident on all forms of imaging.
• Hard-tissue crepitation will be the primary clinical sign of non-inflammatory arthropies.
• Joints with arthropathies can be sub-typed
– Inflammatory or infectious arthropathies
– Post-traumatic degeneration.
– End-stage progression of internal derangements.
– Age-related degeneration
• Patient’s age, degree of pain, difficulty with function, both now and in the future, and perhaps laboratory studies, may influence treatment decisions.
(A screening panoramic film or other imaging with good visualization of the TM joint condyles is desirable but not essential. Condylar change may or may not be apparent in this type.)
The Primary Objective of History and Examination
• Patient age, history and perhaps laboratory studies determine subtype.

Patient Type 8
Aberration in Form
Aberration in form can include congenital or developmental disorders and most are not associated with orofacial pain. They can be categorized as agenesis, hypoplasia, hyperplasia and neoplasia. Hyperplasias and hypoplasias result in facial skeletal asymmetry as well as bifid condyles and other alterations in condylar form. Although often asymptomatic, non-painful deviation or deflection on opening may be seen. The altered form may be congenital, developmental, or secondary to trauma and is usually unilateral. Definitive diagnosis usually requires imaging.
(
A screening panoramic image will be helpful in deciding what other imaging may be indicated.)

|
|





